
I’m the type of person who can hyper focus on things. Often stupid things. Why is the sky blue? What is the real story of that crime I just saw on ID network or did that company on Shark Tank find success? And lately? Will I still be here in a year? Five years? More?
I guess in some weird way I always expected I would live forever. That’s absolutely unreasonable but for some reason my mortality was simply something that never crossed my mind. While others my age (43) were thinking about pre-planning their funeral or preparing a will, I never felt the need. Why would I? I’m never going to die right?
Until the Big ‘C’.
Now it seems like it’s always the first thing I think about when I wake up and the last thing I think about before I fall asleep.
Being a nurse with a terminal diagnosis is a double edged sword. The good thing about it is I either know most of the data or know where to find it. The bad thing about it is I either know most of the data or know where to find it. The problem with metastatic breast cancer is there isn’t really a lot of reliable data to pull from but when you find it, what you find is frightening. Terrifying even.
Tomorrow is my monthly followup with my oncologist. I have spent the past four months avoiding the tough questions. I was too busy simply trying to get back on my feet and not have excruciating pain. I was trying to find a way to have a semblance of a life. It might not be exactly normal, but I could try for as close to it as possible.
I could complain about how unexpected it was, but I guess no one is ever really ready to be told they have incurable cancer. I am trying to deal with it by learning as much as I can about my diagnosis. To arm myself with knowledge.
Tonight I poured over my records trying to understand everything I can about my disease from top to bottom. When I first found out I had an ‘unknown cancer’ on September 25, 2018 the initial thought my doctor had was it was a type of cancer called multiple myeloma which causes cancer cells to accumulate in the bone marrow, where they force out healthy blood cells. Ironically like metastatic breast cancer, multiple myeloma also is treatable but not curable. The five-year survival rate is 48.5%. A daunting number.
I went back for additional testing on September 28th. There were good things to hold onto from those tests. The CT scan of my head showed no masses or lesions. The chest, abdomen, and pelvis CT showed no concerning nodules, masses or opacities in my lungs. My father was diagnosed with metastatic lung cancer in 2015 (at age 64) and died 30 days later after an initial presentation of back pain. Considering what brought me into the emergency room was also back pain, this was at least a little comforting. No masses were seen on my heart, liver, spleen, pancreas, kidneys, gallbladder, uterus or ovaries. None of my lymph nodes were enlarged. On a day of bad news, there was a lot of good to hold onto.
It’s funny. The CT report of my chest, abdomen and pelvis specifically states that ‘multiple punched-out lesions are identified throughout the lumbar spine and bony pelvis. Findings are likely reflective of a primary malignancy such as multiple myeloma. Breast carcinoma would be considered less likely.’ It was considered ‘less likely’ even though it mentioned a ‘questionable speculated lesion in the lateral aspect of the left breast’ and recommended a 3D mammogram. I began my journey believing I had one type of cancer only to be hit with an even worse diagnosis a little over a week later.
I returned for a battery of tests on October 5th. By this time the pain in my back had become so bad that even the car ride to the hospital was more than I could handle. I endured my first mammogram as spasms and waves of pain shot through my body. I think I will have nightmares of this experience until the day I leave this world.
I then had an ultrasound guided breast biopsy with the insertion of a marker clip into the mass in my left breast. They did not fully numb the biopsy site and I literally felt it as each one of the three samples was taken. I then had the pleasure of a repeat mammogram to make sure the marker clip was in the correct place. One mammogram is bad. Two in a day? Torture. My day didn’t end here though. I still had a bilateral iliac bone and bone marrow biopsy to look forward to. Ironically? That hurt much less than the breast biopsy.
 The electronic age can be a blessing and a curse. By the next morning I was able to review the results of my ultrasound on the online patient portal even before I got the dreaded call from my doctor. Tears ran down my face as I read the words ‘suspicious, malignant-appearing mass in the left breast.’ I knew in that moment that I had breast cancer. I also knew what breast cancer that had metastasized to another site meant. It meant stage IV. Terminal.
The electronic age can be a blessing and a curse. By the next morning I was able to review the results of my ultrasound on the online patient portal even before I got the dreaded call from my doctor. Tears ran down my face as I read the words ‘suspicious, malignant-appearing mass in the left breast.’ I knew in that moment that I had breast cancer. I also knew what breast cancer that had metastasized to another site meant. It meant stage IV. Terminal.
When I got off the phone with my new family physician I flashed back to my first appointment with her on August 7th, not even two months before finding out I had cancer. I didn’t go in because I was ill. I’ve always been incredibly healthy in spite of the fact that by all medical definitions I was morbidly obese (235 pounds).
But no. I went in because my physician of eighteen years had left the practice to become the medical director of the local drug treatment facility. I would have never bothered with an appointment had my ONE prescription (lamotrigine for bipolar disorder) not ran out. My new doctor wouldn’t write a new one until she met me and did an initial physical. It didn’t upset me at all. That would be like writing a blank check to someone I never met.
As always the appointment was uneventful. I’m healthy. Until cancer I averaged a visit once every couple years or so and normally only for things like physicals for work or prescription refills. She talked to me about something I hadn’t even thought about. A pap smear. Okay. Full disclosure here. My last one was when my son was born in 1998. Bad nurse. Bad nurse.
We also talked about when I should have my first mammogram. She said that we could think about doing it now if I wanted to, but considering I have no risk factors if I would prefer to wait I could until around age 45. Trust me. I wanted to wait. In retrospect, why didn’t I ask for the darn mammogram? Why did I take the chicken way out? Had I gone in then I could have avoided the horrible pain that led to the emergency room visit on that eventful day. I might have been able to continue working even as I began my treatment.
The breast biopsy confirmed my fears. I had invasive ductal carcinoma with grade 2 cancer cells that don’t resemble normal cells and are growing and dividing a little faster than normal. There are three grades which means mine was middle of the road. Not the best, not the worst. Invasive ductal carcinoma is the most common type of breast cancer and begins in the milk duct then invades the tissue of the breast outside of the duct.
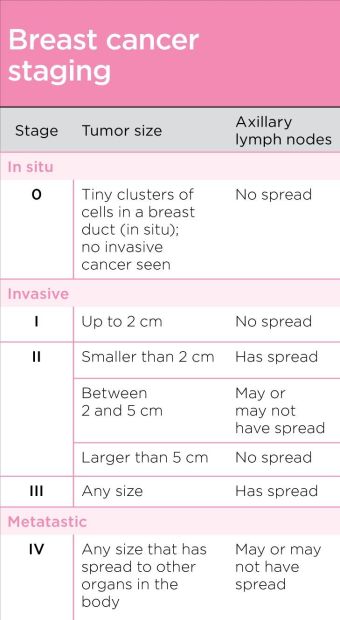
Metastatic breast cancer. As I tried to face those words I thought to myself it must mean the tumor was large. It had to be if it caused the extensive damage it had caused to my bones as it set it’s sights on my spine, pelvis, sternum and right scapula. But it wasn’t big at all. My tumor measured 1.5 centimeters. Only 1.5 centimeters.
If I have metastatic breast cancer that must mean the tumor must have invaded my lymph nodes. But it hadn’t. It hadn’t gotten to my lymph nodes at all. It hopped, skipped and jumped right over my lymph nodes straight into my bones.
The more I read the reports and the more I processed the immense amount of information within them, my mind began racing. I was struck by thoughts that made me angry.
One of the things that upsets me is that I had no family history of breast cancer. Okay I say that with a caveat. My mother was adopted so we have no family medical history on her. However as soon as I was diagnosed with metastatic breast cancer I had genetic testing done. The results of the testing was that I was negative for hereditary cancers including the major breast cancer genes BRCA1 and BRCA2. Apparently I was simply struck by breast cancer lightning.
My tumor was 1.5 centimeters and hadn’t yet invaded my lymph nodes. If it not migrated to my bones it would have been stage I. I could have had surgery and possibly radiation or chemotherapy but there could have been a 100% five-year survival rate. The word ‘remission’ could have been my goal. A cure.
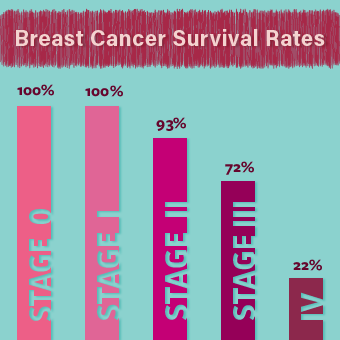
That was not to be for me. Instead it metastasized. Instead it became stage IV. My 100% five-year survival quickly turned into an overall 22%, 36% survival for 15-49 year old women. My best option went from remission and cure to NEAD (No evidence of active disease).
So here I sit. Months later still trying to process the emotions a metastatic breast cancer diagnosis evokes. My best friend keeps telling me to remember I am not a statistic. That life is too short to waste on worrying about statistics and what could happen. My friend told me to remember that I am the patient and not the nurse in this. I need to focus on that.
I wonder if I will ever reach a time when I don’t become terrified the night before my followup appointments. Will I always look over my shoulder or will there come that time when I can take a deep breath and relax? I think the worst part of this diagnosis is the fear of missing out. The fear of what could be.
It’s late. Hopefully I can shut my brain off for a few hours. Good night my loves.
Dx 10/9/2018, invasive ductal carcinoma (IDC), left breast, 1.5cm, Nottingham Grade 2, hormone receptor positive, ER+ (estrogen receptor)/PR+ (progesterone receptor), HER2- (human epidermal growth factor), BRACA- (genetic mutation), Stage IV, metastasized to bones
First CA 27.29 10/9/2018 83 (goal <38)
Hormonal Therapy 10/12/2018 Tamoxifen (Nolvadex, Apo-Tamox, Tamofen, Tamone) pills
Targeted Therapy 10/12/2018 Xgeva (Denosumab) injection
Hormonal Therapy 10/19/2018 Lupron Depot (Leuprolide Acetate) injection
Surgery 11/29/2018 Vaginal hysterectomy with bilateral salpingo-oophorectomy
First CA 27.29 post hysterectomy 12/10/2018 73 (goal <38)
Hormonal Therapy 12/11/2018 Femara (letrozole) pills
Targeted Therapy 12/23/2018 Ibrance (palbociclib) capsules
First CA 27.29 post medication change 1/10/2019 60 (goal <38)

 When you are fighting cancer, you become acutely aware of each and every blood test you take. I’m more familiar with lab values in my five months as a cancer patient than from seven years of nursing. Funny how that works.
When you are fighting cancer, you become acutely aware of each and every blood test you take. I’m more familiar with lab values in my five months as a cancer patient than from seven years of nursing. Funny how that works.
