
It’s been a crazy busy time since I left Kansas for sunny California. I have done my best to live my life without the cloud of cancer hovering over me which is why I have been so radio silent the past three months.
I landed as a palliative care nurse in the beautiful city of San Diego. Considering my own diagnosis, it is a very difficult job for me physically, but more so emotionally. Everyday I am confronted by my own future and I won’t lie, it terrifies me. As hard as it is, I wouldn’t change it for the world. I work with an amazing group of doctors, nurses and social workers. The passion they all have is something I can’t begin to describe.
You might ask, ‘What is palliative care?’ Palliative care provides an extra layer of support by helping patients and families manage pain and other symptoms, offering emotional and spiritual support, comfort care and improved quality of life.
Palliative care really is an amazing resource. I have learned that both as a nurse and as a patient. When you have a life limiting disease, this is something that can make life easier for you and I am so proud to be a part of the outpatient team.
Travel nursing in California was a bucket list item for me. Something new to get outside of the bubble I have always lived in. Can you believe I am 44 and had never lived on my own? Three months in a beautiful city doing the job I love. Walking on the beach and living in an absolutely beautiful home overlooking the mountains. Working with an amazing group of people caring for patients I’ve grown to love. It was like this was meant to be.
San Diego represented a chance at cutting edge cancer care. While I have done my best to live my life here without thinking about cancer, it is and always will be a part of my life. I came to California armed with my medical records and found an amazing medical oncologist at the Scripps MD Anderson Cancer Center.
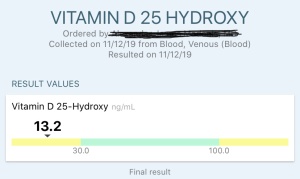
One of the first things she did following my first appointment with her was obtain the pathology slides from my lumpectomy in July so they could do their own testing on it. The results were better than I ever expected. The pathologists here downgraded my tumor from a Nottingham grade 2 to a 1.
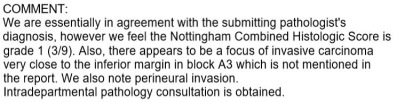
What does that mean for the non-medical people out there? The grade of a breast cancer is a prognostic factor and is representative of the “aggressive potential” of the tumor. In a broad generalization, “low grade” cancers tend to be less aggressive than “high grade” cancers. Determining the grade is very important, and clinicians use this information to help guide treatment options for patients.
A better explanation is:
- Grade 1: Well-differentiated carcinomas have relatively normal-looking cells that do not appear to be growing rapidly and are arranged in small tubules for ductal cancer and cords for lobular cancer. These cancers tend to grow and spread slowly and have a better prognosis (outlook).
- Grade 2: Moderately differentiated carcinomas have features and a prognosis in between these two.
- Grade 3: Poorly differentiated carcinomas lack normal features, tend to grow and spread faster, and have a worse prognosis.
Grow and spread slowly and have a better prognosis. I can’t begin to tell you the relief those words mean to me. In a world filled with uncertainty, hearing those nine words meant everything to me. To be honest, those were the best words I have heard since my diagnosis. September 25, 2018 my world turned upside down and on October 1, 2019, six days after my one year anniversary I received the news that while I still have stage IV breast cancer the prognosis might not be as grim as I initially believed. If that reclassification was the only thing I got from this short three months I would have viewed it as a complete success.
 One of the other things my oncologist at Scripps MD Anderson tested my pathology for was the PIK3CA mutation. The testing came back indicating I am positive for the p.E542K mutation. In other words….. PIK3CA+. This means if/when my current therapy of letrozole and Ibrance fails I at least know what my potential second line of treatment will be. PIQRAY with fulvestrant. While fulvestrant is an injection, after the first month it is only once monthly. PIQRAY is another oral medication. This doesn’t change my treatment today, but it is comforting to have an idea what might comes next.
One of the other things my oncologist at Scripps MD Anderson tested my pathology for was the PIK3CA mutation. The testing came back indicating I am positive for the p.E542K mutation. In other words….. PIK3CA+. This means if/when my current therapy of letrozole and Ibrance fails I at least know what my potential second line of treatment will be. PIQRAY with fulvestrant. While fulvestrant is an injection, after the first month it is only once monthly. PIQRAY is another oral medication. This doesn’t change my treatment today, but it is comforting to have an idea what might comes next.
But that news was tempered with some uncertainty too. My tumor markers have for the most part been pretty spot on with my response to treatment. When my tumor markers went down my PET scan showed the tumor activity was essentially inactive. When they rose in June there was new activity. When I had my last tumor marker before I left for California it was trending down again and had dropped to 46 U/mL.
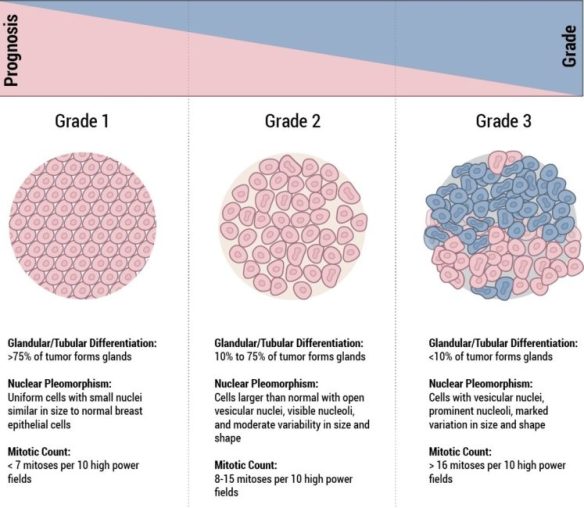
The first result at Scripps a month later was 77.9. This was terrifying. The first thought that crossed my mind was my god, it’s starting again. My oncologist scheduled a PET scan to re-evaluate on October 5, 2019 (a Saturday….they do PET scans on Saturday here!!), but the wait until Monday was almost maddening.
Low level uptake. Those words were like music to my ears. The test was wrong. My followup result on October 25, 2019 went up slightly again to 78.7 U/mL. It still makes me a bit nervous, but like both my oncologist in Kansas and my oncologist here in San Diego have said, the true test is what the scans reflect and symptoms I am feeling. I also have to take into consideration different testing facility, possibly different testing standards which might have an influence on the results. Either way for now I will put that small worry out of my mind.
I am happy to announce that based on my PET scan and my mostly stable tumor markers since I’ve been here, my oncologist has declared me stable! Stable is as close to remission as the metastatic breast cancer world gets. STABLE. What a beautiful word that really is!
Unfortunately the toll a full-time, five day a week with a 40 minute to hour plus commute depending on traffic job has taken on my body has been something I didn’t quite expect. Between the pain in my back that at times isn’t controlled by pain medication and the extreme fatigue I have most days when I come home I am so tired I fall asleep on the couch watching TV or playing a video game.
 My oncologist referred me to the outpatient palliative care clinic for symptom management….the clinic I work for. How ironic, right? It was a little ‘weird’ for my co-workers to treat me so one of the inpatient physicians was awesome and took over my care. Initial course of treatment was Ritalin to help reduce the fatigue.
My oncologist referred me to the outpatient palliative care clinic for symptom management….the clinic I work for. How ironic, right? It was a little ‘weird’ for my co-workers to treat me so one of the inpatient physicians was awesome and took over my care. Initial course of treatment was Ritalin to help reduce the fatigue.
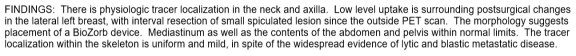
When that didn’t work as well as we hoped, my physician suggested testing my thyroid and vitamin D levels. What do you know? Thyroid is good. A little on the low side of normal, but normal just the same. My vitamin D? Not so much so. Adding vitamin D is helping, but this is a learning process and a work in progress. What I love is the creativity and immense knowledge these doctors have. Who ever would have thought to check these labs? I simply love the palliative care crew!
 The last big development in my world… The ‘R’ word. Radiation. I will be having my radiation sim appointment on Monday after work to plan palliative radiation to my spine to hopefully reduce the pain that I am in most of the time so I am not having to be dependent on pain medication. I hate it and would just like to live a semi-normal life again. I am completely terrified and so alone here right now, but it will be worth it in the end.
The last big development in my world… The ‘R’ word. Radiation. I will be having my radiation sim appointment on Monday after work to plan palliative radiation to my spine to hopefully reduce the pain that I am in most of the time so I am not having to be dependent on pain medication. I hate it and would just like to live a semi-normal life again. I am completely terrified and so alone here right now, but it will be worth it in the end.
The great thing about having radiation here is I will be having it in the same building I work in every day. I can take my lunch break, become happily radioactive and go right back to work. (And for the record…isn’t this an amazingly beautiful facility?) I know my radiation oncologist because I see him everyday in the halls. The thought of radiation in general is terrifying, but a little less scary because the environment is familiar and the doctor is one I know. Honestly, my cancer care from the beginning both in Kansas and here was easier than most people face because I have known all of my doctors prior to becoming their patients. I’m incredibly blessed for that.
Okay…this was much longer than I intended. I guess that is what happens when you don’t do updates for almost three months. I love all of you for the support you have shown me and my family over the past year. My prayer warriors always make me feel loved and very blessed.
I came here to fight. I came here to chase a dream. Never give up, no matter what the odds say!
Dx 10/9/2018, invasive ductal carcinoma (IDC), left breast, 1.5cm, Nottingham Grade 2, hormone receptor positive, ER+ (estrogen receptor)/PR+ (progesterone receptor), HER2- (human epidermal growth factor), BRACA- (genetic mutation), Stage IV, metastasized to bones
Dx reclassified 10/1/2019, IDC, left breast, 1.9cm, Nottingham Grade 1, HR+, ER+/PR+, HER2-, BRACA-, PIK3CA+, Stage IV, metastasized to bones
First CA 27.29 10/9/2018 83 (goal <38)
Hormonal Therapy 10/12/2018 Tamoxifen (Nolvadex, Apo-Tamox, Tamofen, Tamone) pills
Targeted Therapy 10/12/2018 Xgeva (Denosumab) injection
Hormonal Therapy 10/19/2018 Lupron Depot (Leuprolide Acetate) injection
Surgery 11/29/2018 Vaginal hysterectomy with bilateral salpingo-oophorectomy
First CA 27.29 post hysterectomy 12/10/2018 73 (goal <38)
Hormonal Therapy 12/11/2018 Femara (letrozole) pills
Targeted Therapy 12/23/2018 Ibrance (palbociclib) capsules
First CA 27.29 post medication change 1/10/2019 60 (goal <38)
PET Scan 2/22/2019 Breast tumor showed no appreciable FDG uptake (essentially inactive), mets to bone improved from MRI
CA 27.29 5/2/2019 39 (goal <38)
CA 27.29 6/27/2019 53 (goal <38)
PET Scan 6/28/2019 Activity in breast that suggested new or recurrent disease, activity in skeletal lesion appeared to mostly regressed slightly since prior PET scan
Surgery 7/1/2019 Left breast lumpectomy with biozorb placement
First CA 27.29 post surgery 7/25/2019 55 (goal <38)
CA 27.29 8/22/2019 46 (goal <38)
CA 27.29 9/27/2019 77.9 (goal <38.6)
PET Scan 10/5/2019 Low level uptake is surrounding postsurgical changes in the lateral left breast, with interval resection of small spiculated lesion since the outside PET scan. Mediastinum as well as the contents of the abdomen and pelvis within normal limits. The tracer localization within the skeleton is uniform and mild, in spite of the widespread evidence of lytic and blastic metastatic disease.
CA 27.29 10/25/2019 78.7 (goal <38.6)



